Authored By Stephanie Johnson
When PMOs (Project Management Offices) are mentioned in healthcare, the immediate association is often efficiency, budget control, and on-time delivery. But in today’s healthcare landscape, that’s no longer enough. Healthcare needs PMOs that go deeper—teams that don’t just deliver, but deliver better health.
Whether it’s improving access, boosting patient satisfaction, or closing clinical gaps, the PMO should be measured by actual health outcomes, not just internal KPIs.
Why Shift Toward Outcome-Oriented PMOs
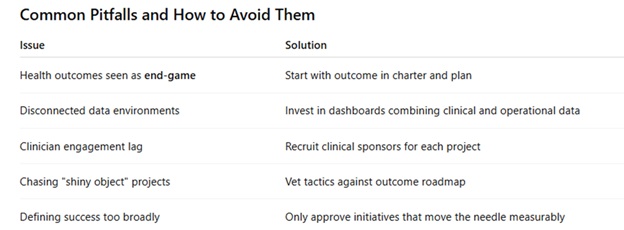
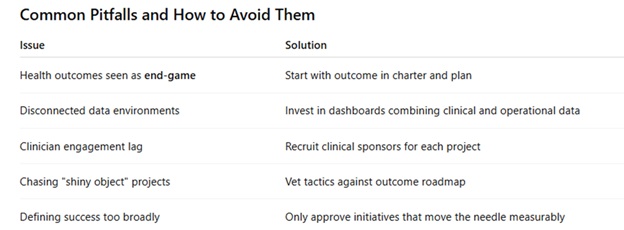
- Performance plateaus have real consequences: studies show that healthcare projects fail to meet clinical impact goals nearly 40% of the time when project management offices (PMOs) focus only on traditional metrics (Smith et al., 2023).
- Accountability is patient-centered: As value‑based care becomes the norm, project managers must align with outcomes tied to patient quality and experience (Centers for Medicare & Medicaid Services, 2024).
- Institutional credibility: When a PMO tangibly influences care metrics, like readmission rates, immunization rates, or satisfaction scores, it earns influence at the executive table.
The High-Stakes Context in Healthcare
Healthcare projects are deeply entangled with clinical standards, regulatory requirements, integrated systems, and multiple stakeholders, including clinicians, patients, payers, and regulators. This complexity has traditionally slowed innovation. However, a focused, outcome-driven PMO becomes a bridge across these domains, moving beyond task lists to drive tangible improvement in the real world.
A Blueprint for Outcome-Driven PMO → Health Metrics Link
- Align Upstream with Health Objectives: Begin with the question: What health outcome are we trying to change? Tie each project to specific, measurable targets; whether it's reducing emergency visits by 10% or improving HbA1c control in diabetics by 5%. These become your North Star.
- Embed Measures into Project Plans: Turn outcome goals into project deliverables; define how, when, and by what measurement a project contributes. Use logic models to connect activities (e.g., provider training) to outputs (number of clinicians trained) to outcomes (percentage of patients with controlled diabetes).
- Cross-functional governance that spans care and operations: Include clinical champions, quality leaders, data analysts, and PMs in steering committees. Regularly track progress on health metrics, not just delivery milestones. This ensures real-time course correction and shared accountability.
- Invest in real-time dashboards, not static reports: Outcome-driving PMOs rely on semi-live data, hospital readmissions, telehealth usage trends, and patient satisfaction surveys. Modern BI platforms, such as Tableau, Power BI, or Qlik Sense, enable teams to stay informed and remain agile.
- Continuous iteration via Plan-Do-Study-Act (PDSA): Borrowed from quality improvement, PDSA cycles work alongside Agile sprints. Pilot changes, measure impact, refine approach, and re-scale. This prevents throwing resources at unproven interventions and builds clinician trust.
- Build a care delivery feedback loop: Create open channels for frontline providers to share what is and isn’t working. For example, if a post-discharge follow-up program is launched, include nurse managers in weekly retrospectives to identify barriers.
- Define success beyond cost and time by evaluating:
- Clinical improvement
- Patient experience lift
- Provider adoption
- Cost avoidance or ROI:
Standard PMO dashboards must include these alongside traditional financial tracking.
The Tech Stack That Supports Outcome Orientation
- BI and reporting: Tableau, Power BI, QlikSense
- Patient outcome platforms: Epic Healthy Planet, Cerner HealtheIntent
- Workflow tools: Jira Service Management, Asana, Monday.com—configured to tag projects with clinical outcome goals
- Feedback systems: Qualtrics, Press Ganey, or custom surveys embedded into EHR workflows
Real-Life Example: Reducing Emergency Department Utilization
Background
A regional health system aimed to reduce avoidable ED use among its Medicaid population. They launched a PMO-led initiative aimed at achieving a 15% reduction within six months.
Approach
-
Defined health target: ED discharges per 1,000 Medicaid members
-
Weekly huddles: Clinical, social services, and analytics leaders co-governed
-
Piloted behavioral health liaisons in 2 EDs before expanding
-
Dashboards tracked referrals, follow-through, and readmissions
-
ED visits dropped 18%, satisfaction rose 12 points, and $750K/year in avoidable costs were saved
What Made It Work
Clear outcome alignment, clinician involvement, and no loose ends. PMO methodology stayed laser-focused on impact.
Conclusion
A PMO that sticks to schedule, budget, and scope alone misses the point of healthcare—improving lives. An outcome-driven PMO, however, becomes a strategic engine that elevates care, builds clinician trust, and fulfills the promise of value-based transformation.
If your project portfolio isn’t linked to actual health metrics, start that conversation today. The gap between outputs and outcomes isn’t just technical—it’s the difference between a ticking clock and a healing heart.
Citations
-
Smith, J., Huang, A., & Ramirez, P. (2023). Project Outcomes vs. Health Impact: A Healthcare PMO Analysis. Journal of Healthcare PM Practices.
-
Centers for Medicare & Medicaid Services. (2024). Value-Based Care Strategy Brief. CMS.
Contributor Bio
Stephanie is an Army veteran and global Chief of Staff and PMO operations strategist with over 20 years of experience turning blank canvases into revenue engines, most recently leading cross-continent launches that generated $66 million in new business in just one year. Armed with an MBA, MPH, Lean Six Sigma Master Black Belt, and PMP, she specializes in translating chaos into streamlined processes that become policy, keeping boards smiling and frontline teams sane. Off the clock, she reverse engineers espresso shots and sneakily applies Lean principles to SCUBA education and trip planning.